A 44-year-old lady presented with stomach pain, heartburn, regurgitation, belching and mid/low dysphagia. She had previously undergone a gastric sleeve procedure in 2015 which was followed by a gastric bypass in 2018.
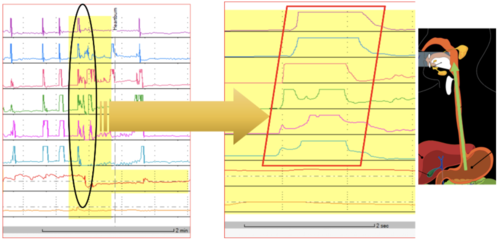
High resolution manometry and 24-hour pH/impedance reflux monitoring was carried out.
High Resolution Manometry
HRM results were as follows:
- The upper oesophageal sphincter was hypotensive and showed complete relaxation on wet-swallows.
- The oesophagus produced normal peristalsis. The patient did perceive dysphagia on solid swallows when failed/weak peristalsis occurred.
- The lower oesophageal sphincter was hypotensive and showed complete relaxation on wet-swallows.
- A 1.8 cm hiatus hernia was observed.
These results based on the Chicago Classification showed that the patient exhibited normal oesophageal motility. There was evidence of a hiatus hernia and hypotensive lower oesophageal sphincter.
24-hour pH-Impedance Reflux Monitoring Off PPI
The pH-impedance reflux monitoring gave the following results:
- Proximal oesophagus: total of zero episodes; norm <31 (impedance).
- Distal oesophagus: total 27.1%, normal 4.2%; upright: 0.2%, normal <6.3%; supine: 46.8%, normal <1.2%; DeMeester score: 90.0, normal <14.72; number of reflux events (impedance); total 9, normal <73 (off PPI).
- Reflux correlations: belching 35 episodes, SI = 14%, SAP = 0%; epigastric pain 1 episode, SI = 0%, SAP = 0%; heartburn 1 episode, SI = 0%, SAP = 0%; positive SI > = 50%, positive SAP >95%.
- Symptoms of regurgitation were not reported during the test.
Pathological acid exposure was seen during the supine period. There was no positive reflux symptom association for belching, epigastric pain and heartburn.
Interpretation
- Gastric acid production was only 18.3% in total (normal > 50% when off PPI) which was compatible with the patient history of gastric sleeve and gastric bypass procedures; this was excluding meal periods.
- Pathological acid exposure at night was mainly due to poor oesophageal clearance with some slow retrograde flow bringing acid up into the oesophagus.
- It was puzzling to note that during the periods of reflux there was not much gastric acid. The patient denied having anything to drink or each at the time.
- During acid exposure time, basal impedance was very slow <200mOhm up to 7 – 9 cm above the lower oesophageal sphincter indicating retention of food materials in the oesophagus.
Next Steps
It was suggested that the 24-hour pH-impedance study be repeated whilst on a full dose of PPI after 8 weeks of treatment. The testing on PPI’s could clarify whether such acid exposure events are indeed responsive to anti-reflux treatment or not as well as investigating refractory symptoms.